The Emergency Room Experience
The first day in the ER was unpleasant, but not horrible. It was Sunday. There were waits, but when we finally were called in, Rosemary was assigned a stretcher and there was a chair where I could sit. We had hoped to avoid the visit, but, after a four-hour stint while the on-call doctor opened his office and confirmed a re-occurrence of her optic neuritis, Rosemary had been sent to the ER for the first of a series of steroid infusions. She couldn’t see enough to read, she had a horrendous headache, high blood pressure, and dizziness.
This was not our first visit to this Emergency Room – the worst being three years earlier when I was the patient. I had tried unsuccessfully to sleep on a stretcher in the aisle next to the nurse’s station for two days and two nights, while I waited for an available room. I swore then that I would die at home rather than go back. But, time wipes out bad memories – mostly fortunately, I suppose. Besides, what choice was there?
After several examinations, many long waits, and an MRI, Rosemary was given her first infusion, and we were allowed to leave, with instructions to go to the doctor’s office in the morning to set up the rest of the infusions – hopefully, at home. Very late that evening, back in our apartment, we collapsed onto the couch, exhausted.
The Vertical Care Room
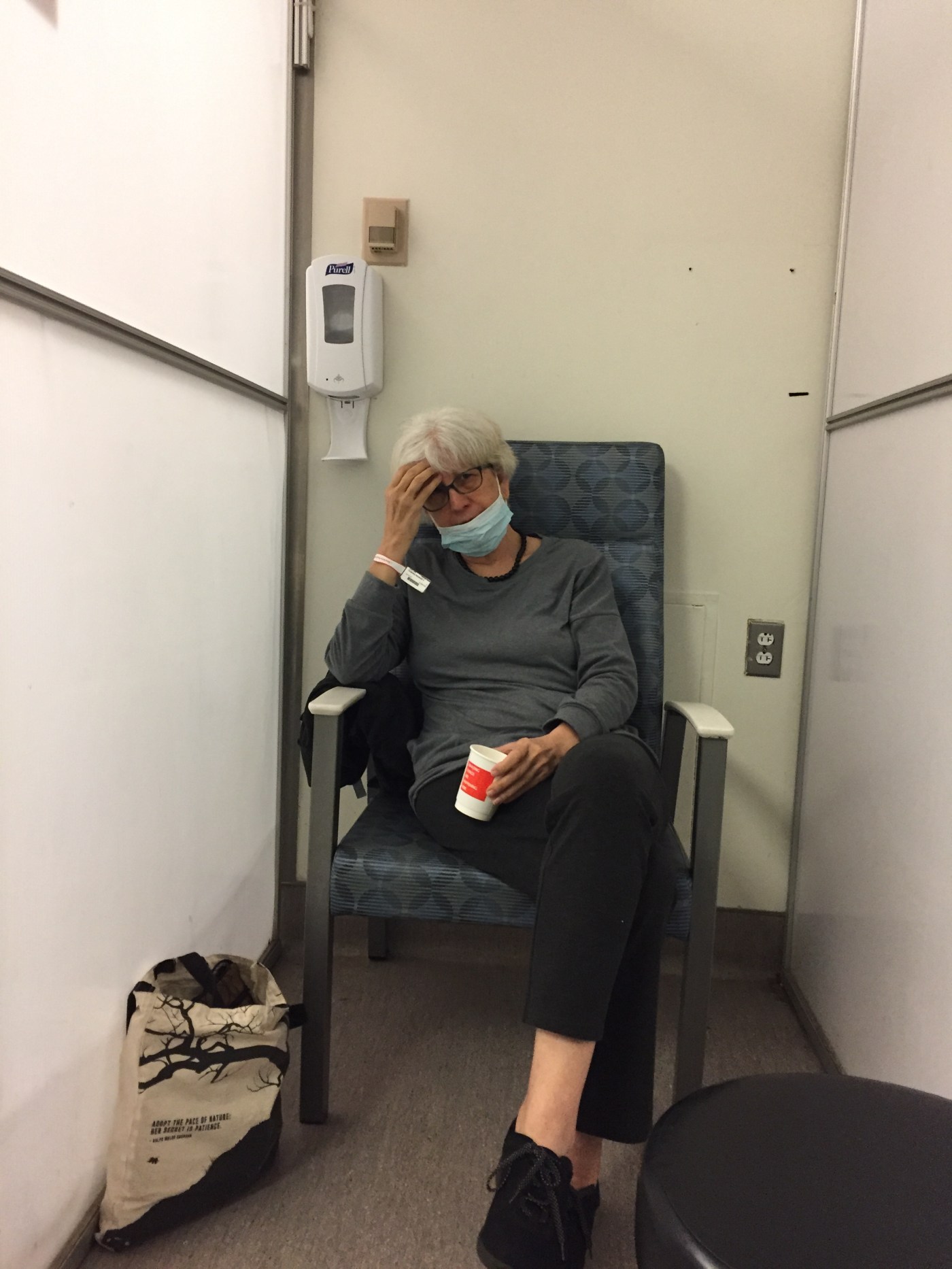
The next morning, the doctor called, sending Rosemary back to the hospital to be admitted. Her flare up was more serious than the last time, and he wanted to take no chances. The second day in the ER was pure hell, made worse by our fatigue from the previous day. Mid-afternoon, Rosemary was assigned to a seat in a small alcove off the hallway, with a sign on the wall that said, “Welcome to The Vertical Care Room.” There, she was given her second steroid infusion.
She sat in a straight-backed chair in a booth, about the size of a telephone booth without the door, just wide enough for her chair, in a line of similar booths. I sat in the hallway, across from her. All the booths were filled with “vertical” patients, meaning they didn’t get to lie down. We commiserated with them and with their visitors. It got more crowded.
I tried to keep my feet out of the narrow space between my chair and the patients in their cubby-hole booths, for there was a steady flow of nurses, visitors, and patients. Everyone talked loudly, trying to be heard over the confusion. There was no privacy, so we learned what each was there for, and often learned more about their bodily functions than we cared to know. Still, when Rosemary’s doctor and his colleague finally came, they stood, in their winter jackets, side by side in the opening to her booth, blocking my view, and I could not hear what they had to say.
Sick people sat in the hallway on hard, straight-backed chairs. One older man (probably younger than I am) sat there for several hours, trying to get someone to let his wife know where he was. Soon, there were not enough chairs for all the patients. One woman was sent to give a urine sample, and when she returned, another patient had taken her seat. She stood, urine sample in hand. I offered her my seat. She was, after all, a patient, and I a visitor. She declined, saying she really didn’t mind standing for a while. She was probably in her twenties, and I am mid-seventies with my own health problems, so I was relieved to keep my seat.
The nurses and medical staff were amazing – kind, patient, telling us whatever they knew, trying to meet patients’ immediate needs. Someone told me later that nurses can work only a short time in the ER before they have to be transferred. One nurse told us that the ER was designed for 60 patients and there were over 170 there that night.
Rosemary had to wait for another MRI which would take about an hour and a half, once she got to the machine. She had been sitting in that booth chair for over ten hours now, and she wasn’t feeling all that well. I needed to go home and rest if I were going to return in the morning, but I wanted to see Rosemary safely lying down. Finally, around 9 pm, I found a nurse and asked if there weren’t some way she could get a stretcher for Rosemary. She studied her computer, looking for options. I told her we were waiting for an MRI.
“When she gets back from her MRI,” she said kindly, “it will be quieter and we will do our best to get her a stretcher. I promise!”
I waited a while and went back. “I know it’s not your job to schedule MRIs, but is there any way you can tell us how much longer we have to wait?”
“I’m sorry. They are scheduled from all over the hospital, so I can’t tell. There are probably over 200 people waiting to get MRIs. If they already came and took her papers, it’s a good sign.”
On my way back to Vertical Care, I saw an older man (again, probably about my age, but I always think I am younger) sitting on the seat of his folding walker in the hallway near the entrance. His wife was on a stretcher across the hall from him, trying to talk to him. They had been there when we came in, many, many hours before. I felt sorry for him, for her.
I waited a while longer. Rosemary looked like she was going to cry. I felt like crying. I didn’t want to leave her sitting in the hard chair with her headache and poor sight. Still, I was struggling with my own health. Rosemary said I should go home. I was crying. She cried. I couldn’t leave. Then I did. I told her to text me when she got a stretcher, even in the middle of the night, so I would see it when I woke up. I told her I would leave my phone on and she should call if she wanted me to come back. I kissed her good-bye and cried all the way home in the taxi. I didn’t sleep well. I had dreams about doctors torturing Rosemary.
Around 1:30 a.m., I got a text message that Rosemary’s MRI was completed, and about half hour later, that she had a stretcher in the ER. I went back to sleep. She told me the next morning that she had cried almost all night, all the way to the MRI and back, and even when she finally had a place to lie down, overcome by the events of the past two days.
The event wasn’t without it’s humorous moments. The next morning, Rosemary suggested I wait to go to the hospital, “until I have a room on the neorealism floor.” I laughed out loud. Clearly an autocorrect. I sent a message to a friend in Rhode Island, “From Vertical Care to Neorealism!” Diane replied, “Hospitals and airlines are in competition for how best to squeeze more and more people into less and less space.”
Single Room, Second Floor – An Oasis
The next morning, I found Rosemary moved to her new floor. Due to an error in the records which showed that Rosemary had the flu, they had put her in a quarantine room, by herself. We had made a trip to the ER two weeks earlier, when Rosemary had indeed been diagnosed with the flu, and they hadn’t taken it off her record.
The new room was the size of a regular hospital room, but with only one bed. The doctors and nurses wore masks with plastic screens over their faces. We breathed a huge sigh to be finally in a place with a bed, a bathroom, a place for me to sit, and some space. We couldn’t believe our good fortune! The meditation chaplain dropped in and offered us about ten minutes of a guided imagery. She was amazing. This place was an oasis. We were so fortunate.
During the day, Rosemary had more tests and more infusions, but when I left at night, I went peacefully, knowing she could finally get some sleep. Rosemary gratefully finally fell into bed, after three days and many, many hours with no sleep. I texted our friend Diane I thought we had moved from Neorealism to Surrealism.
ICU and Step-Down Patients
I showed up the next morning only to learn that after Rosemary had been asleep for a short time, they woke her up at 1:30 a.m. and asked her to change rooms. A woman next door, dealing with addiction, was screaming loudly and needed a single room where she could be with her family. They had discovered that Rosemary no longer had the flu. They were very nice about it, telling her how sorry they were to move her, but there were no choices.
They gave Rosemary some ear plugs and a bed in the hall while they cleaned her room, moved the addicted women into what had been our haven, cleaned the other room, and moved Rosemary into a room she now shared with another. By now, Rosemary’s steroids had kicked in and were contributing to her inability to sleep. Her new roommate was awake and, after a visit, and getting some sleep medication, Rosemary tried again to sleep but she and her roommate were too riled up after all the activity. The roommate was hungry. Rosemary offered her a Kind bar and they talked until morning was near. That roommate left in the morning.
Rosemary spent most of the day in tests and treatment. A new roommate arrived later in the day – a woman just out of surgery and in great pain. She screamed very, very loudly when they moved her onto the bed. Her family members included a man who coughed. Since Rosemary and I both have compromised immune systems, we catch everything and are worried when others around us seem to be not well. To make matters worse, this man conducted business calls. In the room. In the little room where there was barely space for a chair for me to sit on. I went home, hoping that the roommate would calm down after she recovered from her move.
I arrived the next morning to find a still sleepless Rosemary. The second night on the Step Down Unit, her roommate continued to scream. She would stop for a while, Rosemary would drop off, and the screaming would begin again. When I came in that morning, Rosemary was not only wiped out from no sleep, but also anxious about all the chaos, and the steroids were making her talk so fast and long that no one could get a word in!
I tried to visit with Rosemary but could not tolerate being in the same room with the screaming women, even during the day. Rosemary is a person who has great empathy for those around her. In the room, Rosemary’s blood pressure went up. When she went for treatment, where it was quiet, her blood pressure went back to normal. When she went back into her room, her blood pressure went up.
To get some quiet, Rosemary and I left to take a walk and found benches in the hallway. Although the steroids didn’t help, it was primarily hospital conditions that were causing her lack of sleep. I kept looking around for a sofa or someplace where Rosemary might be able to sleep. Rosemary took her pills and the nurses gave her her shots as we sat on the benches.
It became clear that Rosemary was not going to get well in these circumstances. I talked to people in charge of the ward; they were sympathetic, but there were no other rooms. As in the ER, the people who worked here were all terrific – caring, considerate, doing what they could. However, this was a step-down ICU unit, and it was likely that, even if Rosemary did find a quieter roommate, someone coming with similar issues would take the place of the current roommate. After all, Rosemary had dealt with two different screaming women in the past two nights. In the past few months, she had been working very hard to create conditions conducive to dealing with her cancer, another health issue, learning to meditate, to breathe, to stay calm, to avoid stress. I was distressed, but at least I got to go home to sleep.
Shangri-La
We decided to delve into our retirement savings and get Rosemary a private room. There didn’t seem to be an option. Our daughter, Shannon, who lives in California but had been on a business trip in D.C., took the train up to New York. While I took a much-needed break, Shannon helped Rosemary move to her new room on a higher floor.
When I went in the next morning, I stepped into a ward with high, high ceilings, long, wide, empty corridors, a concierge sitting alone behind a big desk in a room bigger than our New York apartment. Sun poured in. Everything was light – and quiet! I found Rosemary in her biggest room yet, all alone. She had slept for the first night since she had been in the hospital. Several chairs, including a lounge chair – which I used for napping – were distributed around the room. A table, where we dined when we were alone, stood in front of the tall window. A refrigerator allowed Rosemary to keep cold food in her room. The bathroom was huge, with a walk-in shower, beautifully tiled; a guest robe hung on the back of the door. The rooms must have had extra sound proofing; it was amazingly quiet. People spoke softly when they came into the rooms.
Here, someone came and quietly asked, “What time would you like to eat?” For the next six days, we enjoyed amazing meals cooked under the supervision of a five-star chef, which we ate in the private dining room when we had guests. (For a very reasonable fee, we could feed our guests.) There were sun-lit lounges that looked out over the East River, where we could watch the boats and barges beneath us and which were supplied with cucumber-infused (or pineapple-infused, or orange-infused) water and ample fruit. There was afternoon tea with the most incredible delicacies – strawberries on brie on a tasty bruschetta, for example. Coffee, tea, several options of gelato, cottage cheese, and other refrigerated treats were in the pantry for guests and visitors.
I was now able to take some breaks as well. When I knew friends were spending time with Rosemary, I stayed home. Finally, I was able to fall apart. On Saturday, I couldn’t get out of bed all day, shades pulled, room dark, unable to read or even watch television. Someone came to the door and I could barely speak to the visitor. I swore once again, that I would die at home rather than endure a stay in the hospital.
Release
The rest of Rosemary’s stay was magic. After eleven days, she went home with her eyesight mostly restored and a cat scan that she was scheduled to do later in the week already completed and with good results.
We both told the story of the hospital stay over and over, to whomever would listen, using words like “shell-shocked” and “traumatized.” We spoke of Dante’s Inferno. Shannon made her partner swear to get her a private room if she ever had to go into a hospital.
We felt survivor’s guilt in the private room, knowing people were probably still sitting in the Vertical Chair Room and trying to sleep with roommates crying in pain. Each time I left the private floor, I was surprised to realize I was still in the same hospital, our circumstances were so different. We were embarrassed at our privilege. Rosemary thought she should tell people she was doing under-cover research on the appalling state of health care in America.
There are many stories of the nightmare of lack of beds and unhealthy hospital situations. There are also stories of health providers who give their all, of caring and smart doctors and nurses, of janitors and maintenance people who made a difference. I don’t think this hospital is unique; friends have told stories of similar experiences at other city hospitals. We ourselves have witnessed this in other hospitals
Our story was an in-your-face example of the inequities of life in America in the 21st century. We were privileged to have retirement funds we could draw on. At least, in our story, Rosemary was able to walk and talk, and, except for the effects of sleeplessness, once she got medicine and treatment, she was not pain-ridden. Thankfully, she had family members who were able to advocate for her.
We are grateful for good doctors and caring nurses, but who is going to pay attention to the need for good hospitals? Rosemary didn’t need such extravagance; she just needed a quiet room and a bed where she could sleep and get the strength she needed to deal with her treatment. A quiet bed to sleep in while she got well.
While I feel like I was living through pieces of this with you as it happened, seeing the entire story in one place is to really see the nightmare. And the horrible inequality in which we are all living. Thanks again, for telling the story so beautifully.
Diane
LikeLike
You did live through much of this with me, Diane, and thank you for letting me vent! It helped a lot.
LikeLike
You got me through a good piece of this drama through your texting. Thanks to you and Diane J and Susan A -who also texted with me-especially through the ER part, I really didn’t feel I was so alone in all this.
LikeLike
This is so horrible, especially the “vertical treatment” areas. WTF? I wouldn’t have lasted two hours in those conditions with my back (and the rest of my body). That is torture for a hospital patient, and shouldn’t even be an option. I’m so disgusted. This makes me determined to go forward with a book on medical trauma and traumatic hospital experiences. I’m so sorry you both went through this. Let me know if there’s ever anything I can do. If you know a social worker, you may want to try getting a patient advocate in advance of another hospital visit, so you have someone to fight for you. I had a bad hospital experience in August, but nothing like what happened here. Then I had difficulty getting medication dispensed that I can die without.
I love you both, and this makes my heart ache so much. This kind of “patient care” should never, ever happen.
LikeLike
Stacy, thank you. Patient Advocate is a good idea! I followed your medicine ordeal and was very upset by it. Unbelievable. I support your idea of a book. More needs to be done about medical care!! Brynna
LikeLike
I am speechless after reading your beautifully written horror story. I’ve been in hospitals in resource countries, and was sadden and shocked by the conditions that sick patients and their family experienced. I now learn that the same inhumane conditions exist in NYC.
Even after experience, your passion for others is present with your understanding that the healthcare workers are helpless in terms of providing a safe, place for healing,
LikeLike
Kerry, And you would know about hospitals, because of your work! And, yes, the people we met were wonderful, they truly cared and tried to do whatever they could under terrible circumstances!
LikeLike
All this when we believe we have the best health system in the world. It does call for an undercover investigation.
It is consoling to know that Rosemary is home and with restored vision and that you, Brynna, don’t need to pull the covers over your head.
Fran
LikeLike
Smiling, Fran. You make me smile.
LikeLike
I am new to your blog and am sorry for your experience. I am intrigued that your previous writer said ” we believe we have the best health system in the world.” Interestingly, it seemed to those of us not living in your country that the so-called “Obama Care” might have brought you up to speed with most of Europe, Canada and Australia, where health care really is about health and not money. Here in Australia, we have private hospitals and private health insurance (neither of which I support, although I have in the past), but you are paying for decor and food and the illusion of choosing your own doctor. Our public hospital system provides everything required for healing and is paid for by our taxation system. As a nurse, I know that hospitals are not the places for rest (unfortunately) and like you, I would rather be at home, but sometimes you need the all the medical stuff to get you on your way. I hope the health issues that plague you and your friend become manageable at home where we all experience the love and rest we need to be truly restored.
LikeLike
Wow, these two points:
“From Vertical Care to Neorealism!”
and
“We both told the story of the hospital stay over and over, to whomever would listen… We spoke of Dante’s Inferno.”
Such a poignant and commanding piece… it really does take you through the illusions of choice in our healthcare system. Your writing skillfully reveals the depths of human emotion that makes this story all the more compelling. This story rekindles my interest in possibly exploring a career health care policy, to effect change.
LikeLike